|
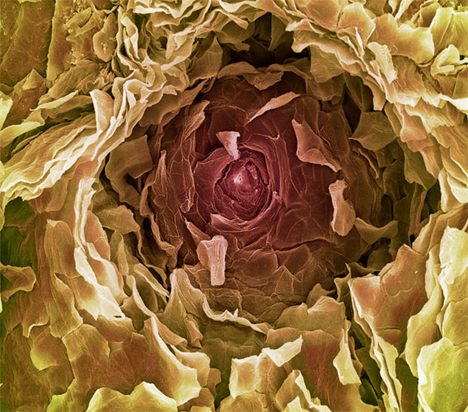
a human sweat gland
For detailed
herbal info on working with fever, check out jim's
online class
Holistic Perspectives in Fever
Fever Phobia

American Academy of
Pediatrics Clinical Report:
Fever and Antipyretic
Use in Children
Janice E. Sullivan, Henry C. Farrar and the Section on
Clinical Pharmacology and Therapeutics, and Committee on
Drugs
Pediatrics; originally published online February 28, 2011
`
www.herbcraft.org/aapfevers.pdf
(this is really worth
printing out to read more thoughtfully, and give to
parents/clients, or to take to pediatric visits to discuss
with your doc)
Some noteworthy quotes (italic emphasis mine):
"Fever, however, is not the primary
illness but is a physiologic mechanism that has beneficial
effects in fighting infection. There is no evidence
that fever itself worsens the course of an illness or that
it causes long-term neurologic complications"
"It should be emphasized that fever
is not an illness but is, in fact, a physiologic mechanism
that has beneficial effects in fighting infection. Fever
retards the growth and reproduction of bacteria and
viruses, enhances neutrophil production and T-lymphocyte
proliferation, and aids in the body’s acute-phase
reaction. The degree of fever does not always correlate
with the severity of illness. Most fevers are of short
duration, are benign, and may actually protect the host.
Data show beneficial effects on certain components of the
immune system in fever, and limited data have revealed
that fever actually helps the body recover more quickly
from viral infections, although the fever may result in
discomfort in children."
"There is no evidence that
children with fever, as opposed to hyperthermia, are at
increased risk of adverse outcomes such as brain damage."
"Studies of health care workers,
including physicians, have revealed that most believe
that the risk of heat-related adverse outcomes is
increased with temperatures above 40°C (104°F), although
this belief is not justified."
"The desire to improve the
overall comfort of the febrile child must be balanced
against the desire to simply lower the body temperature.
It is well documented that there are significant concerns
on the part of parents, nurses, and physicians about
potential adverse effects of fever that have led to a
description in the literature of “fever phobia.” The
most consistently identified serious concern of caregivers
and health care providers is that high fevers, if left
untreated, are associated with seizures, brain damage, and
death. It is argued that by creating undue concern over
these presumed risks of fever, for which there is no
clearly established relationship, physicians are promoting
an exaggerated desire in parents to achieve normothermia
by aggressively treating fever in their children. There
is no evidence that reducing fever reduces morbidity or
mortality from a febrile illness. Possible exceptions
to this could be children with underlying chronic diseases
that may result in limited metabolic reserves or children
who are critically ill, because these children may not
tolerate the increased metabolic demands of fever.
Finally, there is no evidence that antipyretic therapy
decreases the recurrence of febrile seizures."
Fever Literacy and
Fever Phobia
Matthew B. Wallenstein, MD, Alan R. Schroeder, MD,
Michael K. Hole, BA, Christina Ryan, MD, PhD, Natalia
Fijalkowski, BA, Elysia Alvarez, MD, MPH, and Suzan L.
Carmichael, PhD
Clinical Pediatrics; originally
published online 24 January 2013
`
www.herbcraft.org/feverliteracyphobia.html
Some noteworthy quotes (italic emphasis mine):
"This study also demonstrates that
most caregivers (89%) reported that they would give
antipyretics to a comfortable-appearing child with a
fever, and that parents believe the most important use
of antipyretics is for fever, not for pain or
irritability. These additional findings demonstrate
that, despite the laudable attempts of Dr. Schmitt, the
AAP, and others to combat fever phobia, we have made
little progress over the past 3 decades in educating
caregivers regarding the implications of fever, which
may be driving antipyretic overuse and inappropriate
health care utilization.
Our lack of progress
may be iatrogenic. One survey from 1992 found that
65% of pediatricians believe that fever can be dangerous
and that 72% always or often recommend antipyretics to
treat elevated temperatures. However, there is no
evidence that fever, which should be distinguished from
hyperthermia, can cause brain damage. Human body
temperature does not cause physical harm until it
reaches 41°C to 42°C [105.8°F
to 107.6°F]
for a prolonged period of time, which is extremely rare
in infectious conditions.
Recommending
antipyretics to treat elevated temperature is not a
benign intervention for children, particularly when one
half of parents give incorrect doses. Antipyretics
can cause rare but severe side effects, including liver
failure, renal failure, and gastrointestinal ulceration,
and have been associated with Stevens-Johnson syndrome
and asthma. In spite of the evidence, antipyretic use
for febrile children has increased over the last several
decades, from 67% to more than 90%... Our results are
also consistent with a recent study by Enarson et al,
who found that 74% of parents felt that fever was
dangerous and that 90% always attempt to treat fever.
In conclusion,
aggressive educational campaigns for appropriate
antipyretic use should be targeted toward physicians and
nurses.... Given the high incidence of fever in children
and the impact fever phobia has on our health care
system, inclusion of fever and antipyretics on such a
list would be an important step toward changing
behavior."
Myths about Fever
Barton D. Schmitt, MD
`
http://www.rchsd.org/pediatrichousecalls/symptomchecker/feversystoms/fevermythsabout/index.htm
Misconceptions about fever are commonplace. Many parents
needlessly worry and lose sleep when their child has a
fever. This is called fever phobia. Overall, fevers are
harmless. Let the following facts help you put fever
into perspective:
Myth: My child feels warm, so she has a fever.
Fact: Children can feel warm for a many reasons
such as playing hard, crying, getting out of a warm bed
or being outside on a hot day. They are “giving off
heat”. Their skin temperature should return to normal in
10 to 20 minutes. Once these causes are excluded, about
80% of children who feel warm and act sick actually have
a fever. If you want to be sure, take their temperature.
The following are the cutoffs for fever using different
types of thermometers:
` Rectal, ear or temporal artery thermometers: 100.4 F
(38.0 C) or higher
` Oral or pacifier thermometers: 100 F (37.8 C) or
higher
` Under the arm (Axillary or Armpit) temperatures: 99 F
(37.2 C) or higher
Myth: All fevers are bad for children.
Fact: Fevers turn on the body's immune system and
help the body fight infection. Fevers are one of the
body's protective mechanisms. Normal fevers between 100
and 104 F (37.8 - 40 C) are actually good for sick
children.
Myth: Fevers above 104 F (40 C) are dangerous
and can cause brain damage.
Fact: Fevers with infections don't cause brain
damage. Only body temperatures above 108 F (42 C) can
cause brain damage. The body temperature climbs this
high only with extreme environmental temperatures (for
example, if a child is confined to a closed car in hot
weather).
Myth: Anyone can have a febrile seizure (seizure
triggered by fever).
Fact: Only 4 percent of children can have a febrile
seizure.
Myth: Febrile seizures are harmful.
Fact: Febrile seizures are scary to watch, but they
usually stop within 5 minutes. They cause no permanent
harm. Children who have had febrile seizures do not have
a greater risk for developmental delays, learning
disabilities, or seizures without fever.
Myth: All fevers need to be treated with fever
medicine.
Fact: Fevers only need to be treated if they cause
discomfort. Usually fevers don't cause any discomfort
until they go above 102 or 103 F (39 or 39.5 C).
Myth: Without treatment, fevers will keep going
higher.
Fact: Wrong. Because the brain has a thermostat,
fevers from infection usually don't go above 103 or 104
F (39.5- 40 C). They rarely go to 105 or 106 F (40.6 or
41.1 C). While the latter are "high" fevers, they are
harmless ones.
Myth: With treatment, fevers should come down to
normal.
Fact: With treatment, fevers usually come down 2 or
3 F (1 or 1.5 C).
Myth: If the fever doesn't come down (if you
can't "break the fever"), the cause is serious.
Fact: Fevers that don't respond to fever medicine
can be caused by viruses or bacteria. It doesn't relate
to the seriousness of the infection.
Myth: Once the fever comes down with medicines,
it should stay down.
Fact: The fever will normally last for 2 or 3
days with most viral infections. Therefore, when the
fever medicine wears off, the fever will return and need
to be treated again. The fever will go away and not
return once your child’s body overpowers the virus
(usually by the fourth day).
Myth: If the fever is high, the cause is
serious.
Fact: If the fever is high, the cause may or may
not be serious. If your child looks very sick, the cause
is more likely to be serious.
Myth: The exact number of the temperature is
very important.
Fact: How your child looks is what's important, not
the exact temperature.
Myth: Oral temperatures 98.7° to 100°F (37.1° to
37.8°C) are low-grade fevers.
Fact: These temperatures are normal variations. The
body's temperature normally changes throughout the day.
It peaks in the late afternoon and evening. An actual
low-grade fever is 100 F to 102 F (37.8 - 39 C) .
SUMMARY: Remember that fever is fighting off your
child's infection. Fever is one of the good guys.
Fever phobia: misconceptions of
parents about fevers.
Schmitt BD.
Am J Dis Child. 1980 Feb;134(2):176-81.
`
http://www.ncbi.nlm.nih.gov/pubmed/7352443
Abstract Eighty-one parents bringing their children to a
hospital-based pediatric clinic were surveyed about their
understanding of fever. Most parents were unduly worried
about low-grade fever, with temperatures of 38.9 degrees C
or less. Their overconcern was designated "fever phobia."
Most parents (52%) believed that moderate fever with a
temperature of 40 degrees C or less can cause serious
neurological side-effects. Hence, most parents treated
fever aggressively: 85% gave antipyretic medication before
the temperature reached 38.9 degrees C and 68% sponged the
child before the temperature reached 39.5 degrees C. A
review of the literature showed that the only serious
complications of fever were febrile status epilepticus and
heat stroke, two rare entities. The
great concern of parents about fever is not justified.
Health education to counteract "fever phobia" should be a
part of routine pediatric care.
Parental Fever Phobia and Its Correlates
Michael S. Kramer MD1, Lenora Naimark BA1, , Denis G.
Leduc MD1
PEDIATRICS Vol. 75 No. 6 June 1985, pp. 1110-1113
1 The Department of Pediatrics and Epidemiology and
Biostatistics, McGill University Faculty of Medicine,
Montreal
Parents of 202 young febrile children were surveyed about
their knowledge, attitudes, and fears concerning fever and
its treatment. Forty-eight percent of the parents
considered temperatures less than 38.0°C to be "fevers",
43% felt that temperatures less than 40.0°C could be
dangerous to a child, 21% favored treatment for fevers
less than 38.0°C, and 15% believed that, left untreated,
temperature could rise to 42.0°C or higher. Fifty-three
percent advocated waking a febrile child at night to
administer antipyretic therapy. Young age of the child was
associated with a preference for use of acetaminophen over
aspirin and, unexpectedly, with a higher parental
threshold for consideration of fever. The higher their
child's temperature at the time they were questioned, the
higher the minimum temperature that parents considered a
cause for concern. Surprisingly, higher socioeconomic
status was not associated with a lesser degree of fever
phobia. In fact, parents of higher socioeconomic status
were more concerned about the risks of brain damage or
seizures as sequelae of fever than were parents of lower
socioeconomic status. It is
concluded that undue fear and overly aggressive treatment
of fever are epidemic among parents of infants and young
children, even among the highly educated and well-to-do.
Considerable effort will be required on the part of
pediatricians and other child health workers to reeducate
these parents about the definition, consequences, and
appropriate treatment of fever.
Fever Phobia: The Pediatrician's Contribution
PEDIATRICS Vol. 90 No. 6 December 1992, pp. 851-854
Ariane May MD1, Howard Bauchner MD1
1 From the Department of Pediatrics, Division of General
Pediatrics, Boston City Hospital and the Boston University
School of Medicine, Boston, MA.
`
http://pediatrics.aappublications.org/cgi/content/abstract/90/6/851
Fever phobia, the exaggerated fear of fever, is found
among parents of all socioeconomic classes. Pediatricians
may inadvertently contribute to fever phobia if their
practice and educational message are incongruent. To
determine how pediatricians treat fever in their practice,
the authors sent a self-administered questionnaire to a
sample of members of the American Academy of Pediatrics
who lived in Massachusetts. Pediatricians were asked (1)
how dangerous they believed fever to be, (2) how they
treated fever in their practice, and (3) what types of
educational information they gave families regarding
fever. One-hundred seventy-two of the 234 (74%) eligible
pediatricians returned the survey; 151 were completed.
Sixty percent of the respondents were male, and 75%
practiced some form of primary or episodic care.
Ninety-eight (65%) believed that fever itself could be
dangerous to a child, with 58 (60%) of the original 98
citing that a temperature of 104°F or greater could lead
to complications such as seizures, brain damage, or death.
In practice, 108 (72%) always or often recommended
treatment to reduce fever and 96 (89%) of the 108 did so
at temperatures between 101° and 102°F. One hundred
thirty-one (88%) respondents agreed that a sleeping child
with fever should be left undisturbed. One hundred
twenty-one (80%) pediatricians always or often tried to
educate families about fever during sick-child visits, yet
only 38% addressed the dangers of fever. It is concluded
that (1) many pediatricians believe that fever (with no
underlying treatable cause) greater than 104°F could lead
to serious complications and (2) most pediatricians
educate families about fever predominately during
sickchild visits. Pediatricians may
be contributing to fever phobia by presenting mixed
messages to parents about fever—for example, by
prescribing antipyretics for children with temperatures
between 101° and 102°F while recommending that a sleeping
child with fever be left undisturbed and by failing to
address parental concerns about fever during all types of
pediatric visits.
Fever Phobia Revisited: Have Parental Misconceptions
About Fever Changed in 20 Years?
PEDIATRICS Vol. 107 No. 6 June 2001, pp. 1241-1246
Michael Crocetti*, Nooshi Moghbeli*, and Janet Serwint
From the * Department of Pediatrics, Johns Hopkins Bayview
Medical Center, and The Johns Hopkins Children's Center,
Baltimore, Maryland.
`
http://pediatrics.aappublications.org/cgi/content/abstract/107/6/1241
Objectives. Fever is one of the most common reasons that
parents seek medical attention for their children.
Parental concerns arise in part because of the belief that
fever is a disease rather than a symptom or sign of
illness. Twenty years ago, Barton Schmitt, MD, found that
parents had numerous misconceptions about fever. These
unrealistic concerns were termed "fever phobia." More
recent concerns for occult bacteremia in febrile children
have led to more aggressive laboratory testing and
treatment. Our objectives for this study were to explore
current parental attitudes toward fever, to compare these
attitudes with those described by Schmitt in 1980, and to
determine whether recent, more aggressive laboratory
testing and presumptive treatment for occult bacteremia is
associated with increased parental concern regarding
fever.
Methods. Between June and September 1999, a single
research assistant administered a cross-sectional 29-item
questionnaire to caregivers whose children were enrolled
in 2 urban hospital-based pediatric clinics in Baltimore,
Maryland. The questionnaire was administered before either
health maintenance or acute care visits at both sites.
Portions of the questionnaire were modeled after Schmitt's
and elicited information about definition of fever,
concerns about fever, and fever management. Additional
information included home fever reduction techniques,
frequency of temperature monitoring, and parental recall
of past laboratory workup and treatment that these
children had received during health care visits for fever.
Results. A total of 340 caregivers were interviewed.
Fifty-six percent of caregivers were very worried about
the potential harm of fever in their children, 44%
considered a temperature of 38.9°C (102°F) to be a "high"
fever, and 7% thought that a temperature could rise to
43.4°C (110°F) if left untreated. Ninety-one percent of
caregivers believed that a fever could cause harmful
effects; 21% listed brain damage, and 14% listed death.
Strikingly, 52% of caregivers said that they would check
their child's temperature 1 hour when their child had a
fever, 25% gave antipyretics for temperatures <37.8°C
(<100°F), and 85% would awaken their child to give
antipyretics. Fourteen percent of caregivers gave
acetaminophen, and 44% gave ibuprofen at too frequent
dosing intervals. Of the 73% of caregivers who said that
they sponged their child to treat a fever, 24% sponged at
temperatures 37.8°C (100°F); 18% used alcohol. Forty-six
percent of caregivers listed doctors as their primary
resource for information about fever. Caregivers who
stated that they were very worried about fever were more
likely in the past to have had a child who was evaluated
for a fever, to have had blood work performed on their
child during a febrile illness, and to have perceived
their doctors to be very worried about fever. Compared
with 20 years ago, more caregivers listed seizure as a
potential harm of fever, woke their children and checked
temperatures more often during febrile illnesses, and gave
antipyretics or initiated sponging more frequently for
possible normal temperatures.
Conclusions. Fever phobia persists.
Pediatric health care providers have a unique opportunity
to make an impact on parental understanding of fever and
its role in illness. Future studies are needed to evaluate
educational interventions and to identify the types of
medical care practices that foster fever phobia.fever,
fever phobia, child, children, antipyretics, sponging,
health care practices.

Acetaminophen (not just Tylenol) isn't as safe as you
may think...
From a different angle, there is a strong epidemiological
like between the use of Acetaminophen (Tylenol in the
US, Paracetamol in Europe) and asthma. A detailed
article from the American Academy of Pediatricians can
be found here:
The Association of Acetaminophen and Asthma
Prevalence and Severity
John T. McBride
Pediatrics; originally published online
November 7, 2011; DOI: 10.1542/peds.2011-1106
An excerpt:
"The epidemiologic association
between acetaminophen use and asthma prevalence and
severity in children and adults is well established. A
variety of observations suggest that acetaminophen use
has contributed to the recent increase in asthma
prevalence in children:
(1) the strength of the association
(2) the consistency of the association across age,
geography, and culture
(3) the dose response relationship
(4) the timing of increased acetaminophen use and the
asthma epidemic
(5) the relationship between per-capita sales of
acetaminophen and asthma prevalence across countries
(6) the results of a double-blind trial of ibuprofen and
acetaminophen for treatment of fever in asthmatic
children
(7) the biologically plausible mechanism of glutathione
depletion in airway mucosa.
Until future studies document the safety of this drug,
children with asthma or at risk for asthma should avoid
the use of acetaminophen...
...Between 1991 and 1993 the Boston University Fever
Study randomly assigned nearly 84,000 febrile children
aged 6 months to 12 years to receive, as necessary,
low-dose ibuprofen, high-dose ibuprofen, or
acetaminophen (12 mg/kg per dose) in a doubleblind
fashion. Of these children, 1879 with preexisting asthma
were nearly evenly assigned among the 3 groups. For
asthmatic children with a respiratory infection, the
subsequent need for an outpatient asthma visit was 2.3
times higher in those treated with acetaminophen (95%
CI: 1.26–4.16), and the risk was dose-dependent. Because
there was no placebo control, it is theoretically
possible that this outcome was a result of a protective
action of ibuprofen, but the acetaminophen dose
dependence, the lack of dose dependence for ibuprofen,
and the availability of other evidence that
acetaminophen exacerbates asthma make this explanation
unlikely.
`
http://pediatrics.aappublications.org/content/early/2011/11/04/peds.2011-1106.full.pdf
another study found an
epidemiological link between using Acetaminophen to treat
fevers and asthma:
Association between paracetamol use in infancy
and childhood, and risk of asthma, rhinoconjunctivitis,
and eczema in children aged 6—7 years: analysis from
Phase Three of the ISAAC programme
Prof Richard Beasley DSc a , Tadd Clayton MSc b, Prof
Julian Crane MBBS c, Prof Erika von Mutius MD d, Prof
Christopher KW Lai DM e, Prof Stephen Montefort PhD f,
Alistair Stewart BSc g, for the ISAAC Phase Three Study
Group
An excerpt:
"205,487 children aged 6—7 years from 73 centres in 31
countries were included in the analysis. In the
multivariate analyses, use of paracetamol (acetaminophen) for
fever in the first year of life was associated with an
increased risk of asthma symptoms when aged 6—7 years
(OR 1·46 [95% CI 1·36—1·56]). Current use of paracetamol
was associated with a dose-dependent increased risk of
asthma symptoms (1·61 [1·46—1·77] and 3·23 [2·91—3·60]
for medium and high use vs no use, respectively). Use of
paracetamol was similarly associated with the risk of
severe asthma symptoms, with population-attributable
risks between 22% and 38%. Paracetamol use, both in the
first year of life and in children aged 6—7 years, was
also associated with an increased risk of symptoms of
rhinoconjunctivitis and eczema...
Use of paracetamol in the first year of life and in
later childhood, is associated with risk of asthma,
rhinoconjunctivitis, and eczema at age 6 to 7 years. We
suggest that exposure to paracetamol might be a risk
factor for the development of asthma in childhood."
`
http://www.thelancet.com/journals/lancet/article/PIIS0140-6736(08)61445-2/fulltext
And (if that's not distressing enough), Tylenol is just
really decidedly toxic. That's not an
overstatement; it's the most dangerous drug over the
counter in the US (some sources will ciote aspirin, but
aspirin deaths are frequently linked to intentional
suicide attempts, whereas Tylenol/Acetaminophen deaths
are usually unintentional overdoses.
Propublica did a great story; I especially like the
picture oriented tools that allow you to just click on
box labels to see whether you're taking too much
acetaminophen (it's in a LOT more products than
Tylenol):
`
Part 1
`
Part 2
This American Life did a great radio show based off the
Propublica article that you can listen to here:
`
This American Life: Use Only as
Directed

Risks of Fever
Suppression...
Population-level effects of suppressing fever
David J. D. Earn, Paul W. Andrews and Benjamin M. Bolker
22 January 2014 doi:
10.1098/rspb.2013.2570 Proc. R. Soc. B 7 March 2014 vol.
281 no. 1778 20132570
Fever is commonly attenuated with antipyretic medication
as a means to treat unpleasant symptoms of infectious
diseases. We highlight a potentially important negative
effect of fever suppression that becomes evident at the
population level: reducing fever may increase
transmission of associated infections. A higher
transmission rate implies that a larger proportion of
the population will be infected, so widespread
antipyretic drug use is likely to lead to more illness
and death than would be expected in a population that
was not exposed to antipyretic pharmacotherapies. While
the data are incomplete and heterogeneous, they suggest
that, overall, fever suppression increases the expected
number of influenza cases and deaths in the US.
`
http://rspb.royalsocietypublishing.org/content/281/1778/20132570.abstract
A "layperson's" summary of that study can be found here:
Fever Treatments May Cause More
Flu Deaths

Holistic
& Herbal Perspectives on Fever
Holistic Perspectives in Fever
(a 2 1/2 hour online class by herbalist jim mcdonald)
Botanical Medicine in the Stages
of Fever
(paul bergner)
Paul also has an audio recording series that covers a
sensible, energetic treatment of Fevers (and way more)
called Vitalist Treatment of Acute Symptoms; check it
out
here.
©
jim
mcdonald
|

